Shop News
-
25/11/2025Ganoderma Benefits
-
07/02/2025Colds & Flu - treatment and prevention
-
24/01/2025Ginseng - Nature's anti-inflammatory
-
23/01/2025Curcumin Benefits
-
02/05/2024Allergies Tradicional Chinese Medicine
-
12/03/2024Food Combining and Chinese Medicine
-
23/08/2023Phytoestrogens
-
05/06/2023Ginseng Benefits
-
02/06/2023Aumento de precios de la marca Blue Poppy
-
20/07/2022Infertility and Chinese Medicine
-
10/05/2022Allergic Rhinitis
-
24/03/2022TCM Obesity and Its Causes
-
23/03/2022Cancer Prevention and Diet
-
26/01/2022Medicinal Mushrooms
-
18/12/2021Christmas Remedies
-
09/07/2021CANDIDIASIS
-
03/03/2021Chinese Herbal Medicine formula studied to improve cancer therapy
-
12/01/2021The benefits of Xiao Yao San
-
15/09/2020Coronavirus Protocol (summary)
-
01/06/2020TCM Principles for Weight Loss
-
12/02/2020Take Good Care of Your Qi
-
01/01/2020Cordyceps Sinensis Benefits
-
01/12/2019Prevention & Treatment of Colds & Flu
-
27/04/2019ANXIETY - causes and treatments
-
26/03/2019Prostatitis and Chinese Herbs
-
01/03/2019What is an Adaptogenic Herb?
-
05/02/2019New Jade Herbal Formulas
-
09/12/2018The Shen of the Heart
-
23/08/2018Hyperthyroidism and Hypothyroidism
-
05/07/2018FOCUS ON A REMEDY: WARM THE MENSES
-
04/04/2018Treating Insomnia With Chinese Herbal Medicine
-
25/03/2018Cordyceps Sinensis research
-
01/03/2018Chinese Herbal Medicine for Panic Attacks
-
07/11/2017BI SYNDROME
-
01/09/2017Chemotherapy and Anti-Oxidants
-
05/03/2017Lumbar Disc Herniation
-
31/01/2017Treatment Principles in Exterior Invasions
-
21/10/2016Healthy Aging and Oriental Medicine: Qi is the secret
-
23/09/2016Horny Goat's Weed Benefits
-
25/06/2016Ginkgo Biloba Benefits
-
23/03/2016Blood Stasis
-
23/01/2016CHRONIC FATIGUE SYNDROME
-
28/12/2015TONICS
-
24/10/2015A CASE HISTORY OF CHRONIC BRONCHITIS
-
23/09/2015Ganoderma Lucidum reduces obesity in mice
-
01/07/2015The Five Elements and Diet in Chinese Medicine
-
23/05/2015Daoist Sexual Practices
-
21/02/2015DEPRESSION
-
22/01/2015GLAUCOMA
-
20/12/2014ENDOMETRIOSIS
-
28/11/2014POLYCYSTIC OVARY SYNDROME
-
21/08/2014Ear infections and antibiotics
-
24/06/2014FOCUS ON A REMEDY: CHEMO-SUPPORT
-
21/03/2014Stomach-Yin Deficiency and Jade Spring
-
21/02/2014JOY, AN EMOTIONAL CAUSE OF DISEASE?
-
17/01/2014SEXUAL LIFE IN CHINESE MEDICINE
-
19/12/2013ON STAGNATION OF LUNG- AND HEART-QI
-
14/11/2013THREE TREASURES REMEDIES FOR PAIN
-
23/10/2013HEADACHE CASE HISTORY
-
12/07/2013Giovanni Maciocia Clinical Tip: Arouse Power
-
19/04/2013Case history - Chronic constipation
-
18/06/2012Herbs for the treatment of Anorexia
-
09/04/2012REMEDY OF THE MONTH: CLEAR YANG
-
28/04/2011Lingzhi slows progress of Alzheimer’s
-
18/10/2010European Legislation for natural products
-
19/09/2010700-year-old Chinese medicine can treat depression...
-
01/09/2009Swine Flue
Understanding Glaucoma
With an Emphasis on Primary Open-Angle Glaucoma
Introduction
Glaucoma is one of the leading causes of irreversible blindness, with nearly 70 million people suffering from this chronic ophthalmologic condition worldwide. Ninety percent of all cases are primary open-angle glaucoma (POAG). POAG is often called ‘the silent thief of sight’, as in the early disease phase, typically no symptoms are experienced. Patients may experience progressive worsening of their vision, initially peripherally (i.e., vision outside the center of gaze), but eventually involving the central vision. (Vandenbroeck et al 2011)
Primary open angle glaucoma is described distinctly as a multifactorial optic neuropathy that is chronic and progressive with a characteristic acquired loss of optic nerve fibers. Such loss develops in the presence of open anterior chamber angles, characteristic visual field abnormalities, and intraocular pressure (IOP) that is too high for the healthy eye. (Kokotas et al 2012)
Glaucoma is considered as a progressive optic neuropathy often caused by elevated intraocular pressure consequent to abnormally high resistance to aqueous humor (AH) drainage via the trabecular meshwork (TM) and Schlemm’s canal. Morphological and biochemical analyses of the TM of patients with POAG revealed the loss of cells, increased accumulation of extracellular matrix proteins (ECM), changes in the cytoskeleton, cellular senescence, and the process of subclinical inflammation. The TM is the target tissue of glaucoma in the anterior chamber, and the development and progression of glaucoma are accompanied by the accumulation of oxidative damage in this tissue. (Babizhayev MA 2012)
Glaucoma is an optic neuropathy, specifically a neurodegenerative disease characterized by loss of retinal ganglion cells (RGCs) and their axons. In the past, glaucoma was viewed as a disease of raised intraocular pressure (IOP); however, it has become increasingly clear that elevated IOP is only one of the risk factors for this disease. Recent evidence indicates that lowering IOP does not prevent progression in all patients and that progression can continue despite effective lowering of IOP. (Vasudevan et all 2011)
Glaucoma filtering surgery may be compromised by cystic blebs which develop more frequently when anti-metabolites are used to arrest wound healing. Matrix metalloproteinases (MMPs) and the naturally occurring tissue inhibitors of metalloproteinases (TIMPs) are essential in connective tissue remodeling and wound healing. Increased MMPs and TIMPs expression is associated with the formation of filtering blebs, suggesting involvement of MMPs in bleb remodeling. MMP-2 and ProMMP-2 levels in tear fluid may be markers for bleb configuration. (Mathalone et al 2011)
The trabecular meshwork (TM) accounts for about 70–90% of total aqueous humor (AH) outflow from the anterior chamber in the adult human eye. Moreover, the TM constitutes an outflow resistance and thereby determines the intraocular pressure (IOP). Increase of outflow resistance and IOP, eventually, is a major risk factor in primary open angle glaucoma (POAG). POAG patients exhibit specific morphological peculiarities as accumulations of extracellular matrix material (ECM) and condensation or clustering of the cytoskeleton. Frequently, signs of subclinical inflammation are reported. Moreover, deregulations on the cellular level affecting signaling pathways regulating apoptosis, cellular senescence and cell cycle control were observed in ocular cells of POAG patients. (Tourtas et al 2012)
Current glaucoma therapy relies on drugs that lower intraocular pressure (IOP), and several glaucoma medications are effective at lowering IOP when administered properly. However, poor adherence is a fundamental problem that increases with the age of the patient, and approximately 20% of patients eventually require surgery to lower IOP. An alternative treatment approach may lie in the use of neuroprotective agents, designed to promote RGC survival independent of IOP. The most common way to reduce IOP is topical administration of eye drops one or more times daily. (Lavik et al 2011)
There are several classes of effective topical glaucoma medications that lower the IOP. They include prostaglandin analogs (eg, latanoprost), beta-blockers (eg, timolol), alpha-adrenergics (eg, brimonidine), carbonic anhydrase inhibitors (eg, dorzolamide), and cholinergics (eg, pilocarpine). (Lavik et al 2011)
Certain yoga exercises in inverted position (like Sirsasana) leads to two- to three-fold IOP rise from baseline for short duration. We documented a three-fold increase in IOP during the inverted position (IOP checked with Tonopen?) in at least three of our progressive POAG patients with good 24-hour IOP control (personal communication with Dr. Rajul S Parikh). Though evidence is not sufficient to prove the role of inverted yoga exercises as a causal risk factor for glaucoma progression, it is imperative to inform glaucoma patients about IOP elevations associated with inverted posture. (Parikh R & Parikh S)
Blood Tests in Glaucoma
Glucose & insulin – Glaucoma has been positively linked to diabetes mellitus. Glaucoma is more often present in the elderly. Important prognostic factors of glaucoma may be oxidative stress resulting from the toxic effects of glucose, and diabetes-associated vascular complications. Our observations suggest that the generation of reactive oxygen species may promote localized DNA damage in glaucoma-iris tissues of elderly patients vulnerable to diabetic injury. (Szaflik et al 2010)
Homocysteine (Hcy) and hydroxyproline (Hyp) – Increased levels of aqueous humor Hcy and Hyp may be associated with primary open angle glaucoma (POAG). In addition, Hcy and Hyp may be useful protein levels in aqueous humor of POAG patients as a consequence of glaucomatous damage. (Ghanem et al 2012)
hs-C-reactive Protein (CRP) – Measurement of hs-CRP, an inflammatory biomarker, independently predicts future vascular events and improves global classification of risk of cardiovascular diseases. (Shen et al 2012)
Lipid Panel – Serum lipid values could be one of predictable factors in primary open-angle glaucoma diagnosis. Due to the patient age, cholesterol values, as common factors in primary open-angle glaucoma and atherosclerosis genesis, could be concern in the same aetiology based on dyslipidaemia as well. (Pavljasevic & Asceric 2009)
Lipid Panel – The lipid profile exhibited a mild elevation in the patients with POAG. (Su et al 2007)
IL-6 - In glaucoma, the optic nerve head (ONH) is the principal site of initial axonal injury, and elevated intraocular pressure (IOP) is the predominant risk factor. Cell proliferation and IL-6-type cytokine gene expression, rather than astrocyte hypertrophy, characterize early pressure-induced ONH injury. (Johnson et al 2011).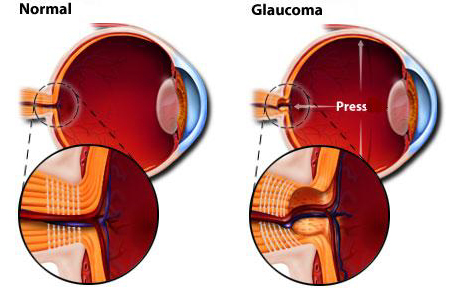 TCM formulas for Glaucoma:
TCM formulas for Glaucoma:
Qi Ju Di Huang Wan
Long Dan Xie Gan Tang
Ming Mu Di Huang Wan
Natural Compounds Helpful in Glaucoma
Anti-oxidants – One factor in the focus of investigative glaucoma research is oxidative stress, as one of the main problems in glaucoma is an imbalance of reactive oxygen species (ROS) formation and decomposition resulting in ROS accumulation, as well as general reduction of anti-oxidant capacities. trabecular meshwork cells were shown to be especially sensitive to oxidative stress, and typical responses affect ECM synthesis, and basic cellular processes, like cell cycle control, proliferation, apoptosis and cellular metabolism. In this respect, prophylactic intake of dietary supplements with alleged antioxidant capacities is recommended for protection from deleterious effects of oxidative stress and prevention of glaucoma thereby. (Tourtas et al 2012).
Ginkgo Biloba extract administration appears to improve preexisting visual field damage in some patients with normal tension glaucoma. (Quaranta et al 2003)
Hyaluronic acid (HA) – is one of the major components of the ECM and may attribute to the filtration function of the trabecular meshwork. The depletion of HA may increase aqueous outflow resistance in the trabecular meshwork of primary open angle glaucoma (POAG) patients. In POAG trabecular meshwork cells, the level of HA concentration increases the activities of MMP-2 and MMP-9. The lack of HA in aqueous humor can result in a reduction in activities of MMPs and therefore may be involved in the pathogenesis of POAG. (Guo & Liang 2012)
Omega-3 Fatty Acids - The stimulation of IL-6, a key pro-inflammatory interleukin and circumscribed oxidative stress marker, was repressed by ?-3 and ?-6, for the former even to a significant extent. Based on the observed side effects of omega-6, omega-3 appears to be the more beneficial fatty acid in respect of prophylactic intake for prevention of a glaucomatous disease. (Tourtas et al 2012)
Vitamin E - The importance of oxidative stress in both the formation and the course of glaucoma has been known. Neuroprotective effects of vitamin E compounds in retinal diseases and glaucoma have been clincally demonstrated. (Engin et al 2010)
